Painless Breakthrough in Diabetes Care: Smarter Monitoring and Drug Delivery
A wearable technology developed by Technion Professor Hossam Haick and colleagues in China enables real-time, non-invasive tracking and optimized treatment for diabetic patients
The researchers recently published their findings in Nature Communications, detailing a wearable platform that enables precise drug dosing through continuous, real-time monitoring of disease and drug markers. Based on microneedles, the system continuously monitors – via the interstitial fluid in the skin – glucose levels and the level of metformin, a common diabetes medication. “This is a new chapter in dynamic, personalized, real-time disease management,” said Prof. Haick.
The interdisciplinary research was led by Prof. Haick of the Wolfson Faculty of Chemical Engineering at the Technion-Israel Institute of technology, Jian Yang, Xia Gong, and Ying Zheng, in collaboration with Prof. Changqing Yi and Prof. Lelun Jiangfrom Sun Yat-sen University in China.
Diabetes is a chronic disease that causes high levels of sugar in the blood, making it difficult for the kidneys to absorb and manage that sugar. It is one of the most common diseases in the world and has been classified by a global epidemic by the UN. According to the Israel Diabetes Association, about 435,000 people in Israel have been diagnosed with diabetes, with an additional 200,000 unaware that they have the disease. In the U.S., according to the CDC, nearly 40 million people – 11.6% of the population – have diabetes. Globally, more than half a billion people are affected.
One of the main challenges in managing diabetes is effectively monitoring both blood glucose levels and the concentration of diabetes medications in the bloodstream. Current technologies are invasive, painful, and unable to provide continuous updates as the body’s physiological conditions change. Most treatments follow a one-size-fits-all approach that does not account for individual differences in metabolism, drug absorption, and response. This lack of precision can lead to dangerous conditions such as hypoglycemia (extremely low blood glucose levels).
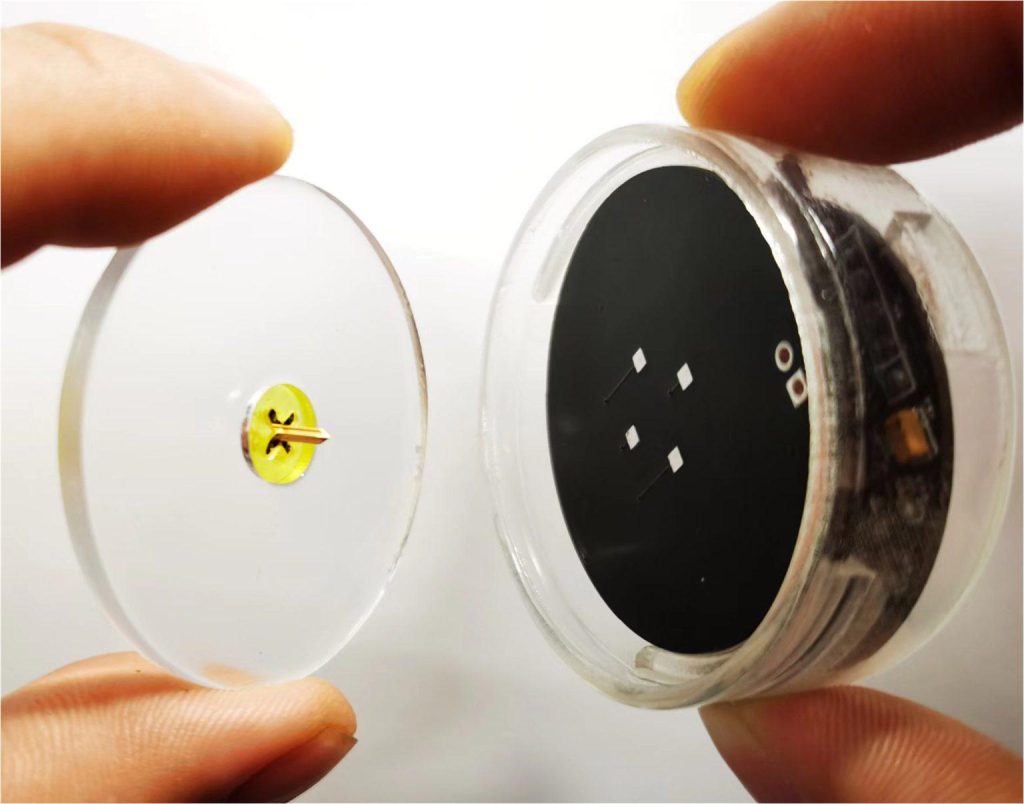
The research team’s new technology solves these problems through continuous monitoring of biological markers and medications using an array of microneedles, which adheres to the skin without causing pain and monitors glucose and drug levels in real time. The platform system combines 3D-printed microneedles, nano-enzyme-based sensors, smartphone connectivity, and a dedicated app that enables pharmacologically guided diabetes treatment.
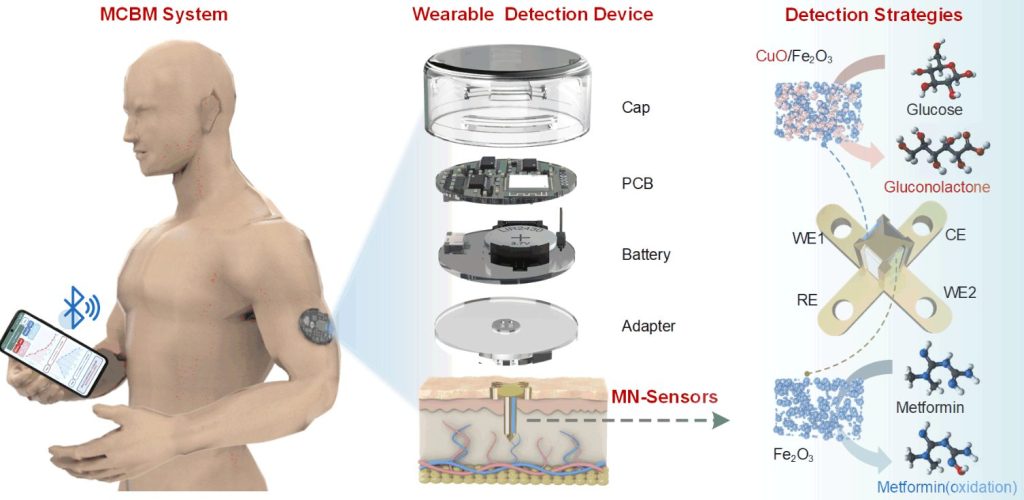
It operates as a closed loop: the microneedles penetrate the upper skin layer and monitor biomarkers found in the interstitial fluid. Using unique sensors containing nano-enzymes, the system continuously and accurately measures glucose and metformin levels. The signals are transmitted via Bluetooth to a mobile phone app, which performs real-time pharmacokinetic (PK) and pharmacodynamic (PD) analyses and generates personalized drug profiles and dosage recommendations. The app alerts users or caregivers immediately to any significant changes.
The researchers validated the system both in laboratory conditions (in vitro) and in animals (in vivo). In a study with diabetic mice, the system’s results showed a strong correlation with conventional methods (such as ELISA and glucose meters). Moreover, the new system detected fluctuations in glucose and drug levels that existing systems missed. The researchers did more than just demonstrating the system’s effectiveness – they also used it to build personalized pharmacokinetic models, showing how the same dose of metformin affected different individuals differently, depending on factors such as age, weight, and metabolism. The system enables dose optimization, balancing treatment effectiveness with safety, especially in preventing lactic acidosis – a complication that can cause dizziness, vomiting, fatigue, muscle cramps, hallucinations, and even liver failure.
“Through continuous monitoring of both the disease state and the treatment agent, the system allows unprecedented real-time control of treatment,” said Prof. Hossam Haick. “It opens new avenues not only for diabetes but also for any chronic disease that depends on a narrow therapeutic window. The compact and user-friendly system is therefore suitable for personalized, real-time disease management. This innovation aligns with the vision of smart medicine that combines wearable biological sensors, artificial intelligence, and pharmacology.”
In the future, the team aims to expand the system to monitor other chronic conditions, such as heart disease or epilepsy, by adjusting the sensing chemistry. According to paper co-author Prof. Changqing Yi, “This work brings us closer to an era where wearable devices will not only tell you what’s happening in your body but will also guide your treatment in real time.”
For the full article in Nature Communications









