Could a Living Implant End Daily Insulin Injections?
Groundbreaking research reveals a self-regulating, implantable living technology that could offer hope for millions with diabetes and other chronic diseases
A pioneering study led by Assistant Professor Shady Farah of the Faculty of Chemical Engineering at the Technion – Israel Institute of Technology, in co-correspondence with MIT, and in collaboration with Harvard University, Johns Hopkins University, and the University of Massachusetts, marks a major step toward eliminating the need for daily insulin injections for people with diabetes.

The research introduces a living, cell-based implant that can function as an autonomous artificial pancreas, essentially a living drug that is long-term, thanks to a novel crystalline shield-protecting technology. Once implanted, the system operates entirely on its own: it continuously senses blood-glucose levels, produces insulin within the implant itself, and releases the exact amount needed – precisely when it is needed. In effect, the implant becomes a self-regulating, drug-manufacturing organ inside the body, requiring no external pumps, injections, or patient intervention.
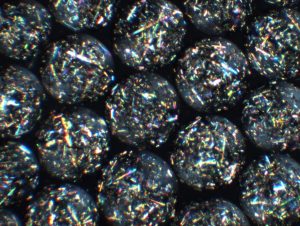
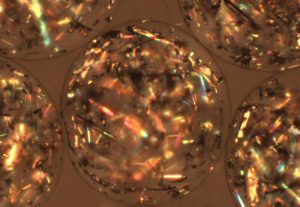
One of the study’s most significant breakthroughs addresses the longstanding challenge of immune rejection, which has limited the success of cell-based therapies for decades. The researchers developed engineered therapeutic crystals – called “crystalline shield” – that shield the implant from the immune system, preventing it from being recognized as a foreign object. This protective strategy enables the implant to function reliably and continuously for several years.
The technology has already been successfully tested in a mouse model for effective and long-term regulation of glucose levels and in non-human primates for cell viability and functionality. These results represent a critical milestone and strongly support the potential for future translation to human patients.
From Postdoctoral Insight to Global Collaboration
Asst. Prof. Farah began developing the concept with colleagues in 2018 during his postdoctoral fellowship at MIT and Boston Children’s Hospital/Harvard Medical School, under the supervision of Prof. Daniel Anderson and Prof. Robert (Bob) Langer, a world leader in tissue engineering and co-founder of Moderna.
Today, the research continues in Asst. Prof. Farah’s laboratory at the Technion, in close collaboration with leading U.S. institutions, including MIT, Harvard, the University of Massachusetts, Boston Children’s Hospital, and the Johns Hopkins University School of Medicine.
A Platform with Far-Reaching Potential
While the immediate focus is diabetes, the researchers emphasize that this implantable, closed-loop platform could be adapted to treat a wide range of chronic conditions requiring continuous delivery of biological therapeutics – including hemophilia and other metabolic or genetic diseases.
If successfully translated to the clinic, this technology could redefine how chronic diseases are treated, shifting from repeated drug administration to living, self-regulating therapies that work seamlessly from within.
The paper’s equal co-first authors are Matthew Bochenek (MIT), Shady Farah (and Co-corresponding author) Joshua Doloff (JHU). Also involved with this study are members of the Farah lab at the Technion: co-authors Dr. Merna Shaheen-Mualim and former master’s students Neta Kutner and Edwar Odeh (currently a researcher on the team). The work earned the prestigious front-page cover of Science Translational Medicine on January 28 (Credit: Shady Farah and adapted by Maya Levi and Edwar Odeh).
To read the full article, click here