“I Told My Father That the Technion Is My Place”
In honor of the International Day of Women and Girls in Science, meet Hiba Mallak, a Dean’s List honoree at the Henry and Marilyn Taub Faculty of Computer Science

In honor of the International Day of Women and Girls in Science, meet Hiba Mallak, a Dean’s List honoree at the Henry and Marilyn Taub Faculty of Computer Science

An innovative technology developed by Assistant Professor Ofer Berman of the Technion and researchers at Cornell Tech offers passive air cooling without electricity and without pollution

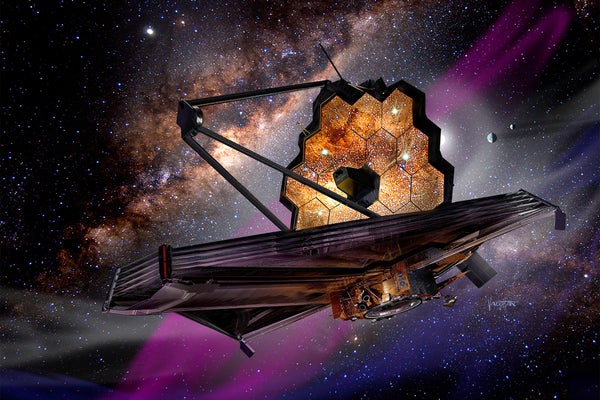
Technion-led team achieves first measurement of cosmic rays deep inside star-forming nebula 400 light-years from Earth

Technion on the Bar - When Waste Meets Recycling
17.02.2026 Tuesday, at 20:00
Add to calendar

The Second Israeli Conference on the Philosophy of Artificial Intelligence
04.03.2026 Wednesday, at 09:30
Add to calendar

Nature on Campus Photography Exhibition
04.01.2026 Sunday, at 09:00
Add to calendar
Landmarks Exhibition
01.01.2026 Thursday, at 09:00
Add to calendar
15000
Students
in a variety of degrees
60
Research Centers
across campus
18
Faculties
100000
Graduates