Immunology & Reward
Researchers at the Technion have successfully shrunk cancerous tumors in mice by manipulating the brain’s reward system. The explanation: the intervention caused the nervous system to stimulate the immune system.
Artificially activating the brain’s reward system has led to a dramatic reduction in the size of cancerous tumors in mice. This is the conclusion of a study conducted at the Technion and published in the journal Nature Communications. The research was led by doctoral students Tamar Ben-Shaanan and Maya Schiller, under the supervision of Assoc. Prof. Asya Rolls of the Technion Rappaport Faculty of Medicine and Technion Asst. Prof. Fahed Hakim, Medical Director of the Scottish EMMS Hospital in Nazareth.
The immune system’s natural ability to destroy cancer cells has become increasingly clear in recent years. This has led to the growth of immunotherapy – an innovative medical approach based on the understanding that the immune system is able to fight cancer effectively if given the tools. In 2013, the editors of the journal Science called immunotherapy the most important breakthrough of the year. “However,” explains Prof. Rolls, “the immune cells’ involvement in cancerous processes is a double-edged sword, because certain components in these cells support tumor growth. This is done by blocking the immune response and creating an environment that is beneficial to growth.”
Prof. Rolls has been studying the brain’s effect on the immune system for several years. In a study she published in 2016 in Nature Medicine, she showed how the immune system can be stimulated by manipulating the brain’s reward system – which operates in positive emotional states and in anticipation of the positive. She says, “By artificially activating the region, we can affect the nervous system and, in turn, the immune system.” In the same article, Prof. Rolls and her colleagues showed that artificial intervention sends messages to the sympathetic nervous system, which stimulates the immune system. Moreover, as a result of the intervention, the immune system created a stronger immune memory against the bacteria to which it had been exposed, therefore it will work more efficiently the next time it is exposed to the same bacteria.
Most immune cells come from the bone marrow – the spongy tissue found in bones. The brain communicates directly with bone marrow, and can affect its attributes. The main breakthrough in this study is the researchers’ success in harnessing the immune system and preventing the cancerous tumor from taking over. The result is a dramatic contraction of the cancerous tumor in response to the activation of the brain reward system.
“The relationship between a person’s emotional state and cancer has been demonstrated in the past, but mainly in relation to negative feelings such as stress and depression and without a physiological map of the action mechanism,” Prof. Rolls said. Several researchers, for example, Prof. David Spiegel of the Stanford University School of Medicine showed that an improvement in the patient’s emotional state may affect the course of the disease, but it was not clear how this happened. We are now presenting a physiological model that can explain at least part of this effect.”
According to Prof. Hakim, “Understanding the brain’s influence on the immune system and its ability to fight cancer will enable us to use this mechanism in medical treatments. Different people react differently, and we’ll be able to take advantage of this tremendous potential for healing only if we gain a thorough understanding of the mechanisms.”
The authors pointed out that the study is preclinical and that they tested only two cancer models (melanoma and lung cancer) and only two developmental aspects – tumor volume and weight. However, this breakthrough will allow doctors to realize the physiological role the patients’ mental state may play in the development of malignant diseases. By artificially activating different parts of the brain, in the future it might be possible to encourage the immune system to block development of cancerous tumors more effectively.
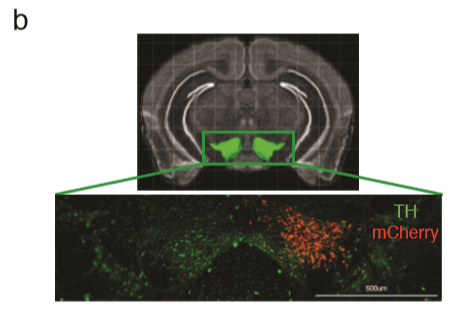
Image of the reward system (VTA). Experimental mice were injected with a special compound known as a DREADD, that allows researchers to manipulate the brain and activate the reward system. The red is the DREADD expression limited to the reward system;
“I want to emphasize what our findings do not say,” Prof. Rolls said. “They do not say that it is applicable for all types of cancer and most importantly that it is not applicable to humans at this point. It is a robust artificial type of manipulation, designed to determine the system’s potential. In real-life situations, it most probably works differently, especially because other systems are also involved. For example, stress may counteract these reward system effects. I think it’s crucial for people to know that it’s not that one can just think positively and get better. People are very different in their reactions, and until we fully understand how this works, it merely offers a potential.”
The work was supported by the Adelis Brain Research Award. The Adelis Foundation was established by the late André Cohen Deloro to support academic excellence in Israel, in particular within the realm of medical and scientific research. In 2015, in line with Deloro’s legacy and vision, the Foundation inaugurated the Adelis Brain Research Award and the winner receives a $100,000 research grant. The prize is intended to encourage excellence in the field of brain research in Israel and to translate the research into global impact for the benefit of all humanity
Assoc. Prof. Asya Rolls completed her bachelor’s and master’s degrees at the Technion’s Faculty of Biology, and after her doctorate at the Weizmann Institute of Science and post-doctorate at the Department of Psychiatry at Stanford University in California, she joined the Technion’s Rappaport Faculty of Medicine in 2012 as a faculty member. She was awarded the Adelis Brain Research Award, the Krill Prize, a European Research Council Grant, elected to the Israel Young Academy of Sciences and the FENS-Kavli Network of Excellence, and recognized as one of 40 international researchers by the Howard Hughes Medical Institute (HHMI).
Clinical Asst. Prof. Fahed Hakim was recently appointed Medical Director of the Scottish EMSS Hospital in Nazareth and continues to serve as a Senior Physician at the Pediatric Lung Institute at the Rambam Health Care Campus in Haifa. Prof. Hakim is an expert in pediatrics, pediatric pulmonology, and sleep disorders. He is an active member of the international associations for the study of lung disease, sleep, and brain research respectively. After completing a postdoctoral fellowship at the Department of Sleep Research at the University of Chicago in Illinois in 2013, he joined the Technion’s Rappaport Faculty of Medicine as a faculty member.